Vitamin D Deficiency And Intrusive Thoughts
Vitamin D Deficiency And Intrusive Thoughts
Definition/Description [edit | edit source]
Vitamin D deficiency is a major public health problem worldwide in all age groups causing adverse effects on skeletal health and other health consequences. Even in countries with low latitude, where it was generally assumed that UV radiation was adequate enough to prevent this deficiency, and in industrialized countries, where vitamin D fortification has been implemented now for years vitamin D deficiency is still a major problem.[1]
Vitamin D regulates and modulates the physiology and function of multiple human systems, including the skeletal muscle[2]. It is a necessary vitamin for calcium absorption, maintaining serum calcium and phosphate concentrations to enable normal mineralization of bone, and to prevent hypocalcemic tetany. It is also needed for bone growth and bone remodelling by osteoblasts and osteoclasts.
Inadequate amounts of vitamin D is most commonly associated with rickets in children and osteomalacia in adults, where bones soften and loose integrity. Serum levels less than 20 mg/mL are considered deficient.[3]
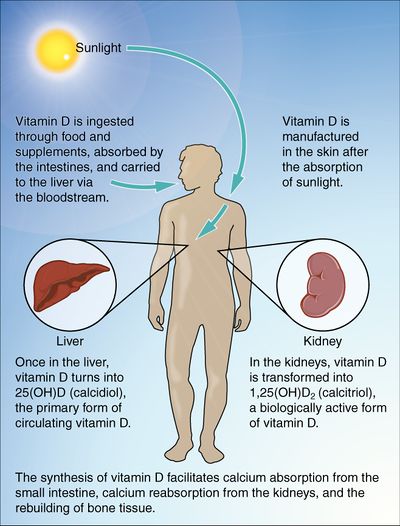
Vitamin D, also known as calcidiol or 25(OH)D, is a fat-soluble vitamin obtained from sun exposure, food, and supplements. It is not naturally present in many foods but is often used to fortify food or taken as a dietary supplement.Vitamin D is synthesized in the body when cholesterol[3] (7-dehydrocholesterol)[4] activates with UVB rays from sunlight. When ingested, the intestines absorb the vitamin and send it to the liver and kidneys for further processing.
Prevalence [edit | edit source]
Vitamin D deficiency is a major public health problem worldwide in all age groups.[1]
Low vitamin D status is a problem even in countries with sun exposure all year round. This problem is particularly high in the Middle East, specially among girls and women[1].
A minimum of 25% up to 50% US adult population are vitamin D deficient.[5] [6] According to a recent National Health and Nutrition Examination Survey, overall prevalence rate of vitamin D deficiency is approximately 41% in the US adult population. Regarding ethnicity, deficiency is most commonly seen in African Americans followed by Hispanics.[5] UVB rays are absorbed by the melanin in people with darker skin tones; therefore, having a significant reduction of synthesis.[7]
Risk Factors [edit | edit source]
- Geriatric population[4] [7]
- Infants[3]
- People with limited sun exposure[3]
- Fat malabsorption[3]
- Obesity (all ages)[8] [9]: fat soluable vitamin is easily stored in adipose tissues --> decrease vitamin D in bloodstream[7]
- Gestational diabetes[10]
- Poor general health status[5]
- Hypertension[5]
- Insufficient daily intake of milk or other vitamin D containing foods[5] [11] [3]
- Depression[12]
- Burn patients[13]
- Living in polluted climates[3]
Deficiency may be linked to geographic location and religious practices, but evidence for this is inconsistent.[3]
Possible causes- Northern countries have little exposure to sunlight; Clothing covering major surfaces of the body year-round such as with Arab women[4]
Characteristics/Clinical Presentation [edit | edit source]
Adults generally present with the diagnosis of osteomalacia, which may include the following signs and symptoms[4] [3] [14]:
- General muscle weakness
- Falls
- Fractures
- Severe bone pain
- Myalgia
- Decreased functional status
- Decreased progress during rehabilitation
- Fatigue
- Depression
Children typically present with rickets as their diagnosis, which may include the following signs and symptoms[4]:
- Bowing of the long bones
- Widening, fraying, and clubbing in areas of active bone growth, predominantly around the metaphyseal ends of the long bones and sternal ends of the ribs.
Associated Co-morbidities [edit | edit source]
Osteoporosis [4]
The hormone 7-dehydrocholesterol decreases in the skin as a person ages. By age 65, approximately only 25% of it remains in the body, leading to decreased synthesis of vitamin D and therefore calcium absorption.
Skeletal Deformities[4]
In children with rickets there is often bowing of the long bones and widening, fraying, and clubbing near epiphyseal (growth) plates. Predominant areas include metaphysis of the long bones and sterna ends of the ribs, which is also known as rachitic rosary.
Electrolyte Imbalance [4]
Often associated with hypomagnesemia
Hyperparathyroidism
Parathyroid hormone (PTH) is a key hormone that regulates renal synthesis of calcidiol or 25(OH)D, which therefore maintains calcium ions in the blood. Low levels of vitamin D (calcidiol) and calcium ions in the blood stimulate the PTH. Through this mechanism, the active vitamin D metabolite [1,25(OH)2D], also known as calcitriol, promotes calcium supply to the bloodstream. As the cascade progresses, parathyroid is overstimulated, causing secondary hyperparathyroidism.[7] [11]
Cancer
Vitamin D may play a role in the prevention of colon, prostate, and breast cancers. Due to vitamin D receptors' presence in colon, prostate, and breast tissues, vitamin D receptors often play a role in the proliferation of cells and their response to various stimuli.
The lack therefore may indicate possible increase of cancer risk.[7]Research is often conflicting in this area.[3]
Myofascial Trigger Points/Myalgia [4]
Other potential comorbidities [3]
Diabetes (type I and II), Insulin Intolerance, Hypertension, Multiple Sclerosis, and decreased cognition as seen in Alzheimer's disease[14]
Medications [edit | edit source]
| Medication | Effect |
| Anticonvulsants: (phenytoin, carbamazepine, Phenobarbital) | Induce hepatic p450 enzymes to accelerate the catabolism of vitamin catabolism of vitamin D29 |
| Thiazide diuretics | Metabolized by hepatic p450 enzymes, can accelerate the catabolism of vitamin D |
| Corticosteroids | Metabolized by hepatic p450 enzymes, can accelerate the catabolism of vitamin D |
| Nicotine | Metabolized by hepatic p450 enzymes, can accelerate the catabolism of vitamin D |
| Cholesterol-lowering medications: (Cholestyramine, colestipol, ezetimibe) | By blocking the absorption of lipids in the intestines, these medications also block the absorption of vitamin D and other fat-soluble vitamins |
| Cimetidine | Metabolized by hepatic p450 enzymes, can accelerate the catabolism of vitamin D |
| Heparin | Metabolized by hepatic p450 enzymes, can accelerate the catabolism of vitamin D |
| Diet agents (xenical, Alli) | While blocking the absorption of fat in the intestines, this medication also blocks the intestines, this medication also blocks the absorption of vitamin D and other fat-soluble vitamins |
Diagnostic Tests/Lab Tests [edit | edit source]
A risk marker used to measure defficiency levels is the plasma metabolite of Vitamin D, 25-hydroxyvitamin D (25(OH)D)[6] [11]
Various methods available to measure 25(OH)D concentration include[11]:
- Competitive Protein Binding Assay (CPBA)
- Radioimmunoassay (RIA)
- Enzyme-linked Immunoassay (EIA, ELISA)
- Random Access Automated Assay using chemiluminescence technology (RAAA)
- High-Performance Liquid Chromatography (HPLC)
- Liquid Chromatography-mass Spectrometry (LC-MS)
- 24-hour Urine Calcium Excretion[6]
Radiographs of patients with vitamin D deficiency typically show:Decalcification in the spine, pelvis, and lower extremities; Transverse fracture-like lines in the affected bones; Demineralization of bone matrix[4]
Etiology/Causes [edit | edit source]
Adults [edit | edit source]
Primary causes include: inadequate sun exposure[4], insufficient supplementation, pregnant/lactating, and obesity.[7]
Children and Adolescents [edit | edit source]
Main causes include: inadequate sun exposure[4], inadequate vitamin supplementation, and breastfeeding without vitamin D supplementation.[7]
Other Causes
- Low intake of vitamin D in diet[4]
- Poor renal function: reduces conversion of 25(OH)D to active metabolite in kidney[11]
- Intestinal malabsorption problems, often associated with ageing[4]; Irritable Bowel Syndrome (IBS)[7]
- Long-term uses of anticonvulsants (see relevant section in link), which accelerates breakdown of the active forms of vitamin D[4]
- Autoimmune disorders: helper T cells (Th), a key componenet to antigen-specific immunity, is misdirected. Th cells (1 and 2) have vitamin D receptors on them, which assist in suppressing the autoimmune disease --> vitamin D cannot bind with misdirected Th cells and also cannot assist in suppression of the disease (cyclic)[7]
Systemic Involvement [edit | edit source]
- Musculoskeletal System: Severe vitamin D deficiency may be associated with non-specific musculoskeletal pain, causing bone, muscle, and/or joint pain.[15] [16] When there is a vitamin D deficiency present, there is lack of suppression of autoimmune disorders, through Th1 cells. Common autoimmune disorders may include: RA and MS.[7] Also, there are vitamin D receptors on skeletal muscle. When deficiency present, there is an associated increased risk of falls.[7]
- Endocrine System: Secondary hyperparathyroidism[11] [7]
- Cardiovascular System: Research suggests that low vitamin D may be a risk factor for certain arterial diseases such as Peripheral Artery Disease, Congestive Heart Failure, and Aortic Aneurysms.[17] [18] It may also contribute to decreased protection over lung function and increase lung functional decline in smokers.[19] Vitamin D may have an affect on cardiac contractility, vascular tone, and cardiac tissue maturation due to the vitamin D receptors on the heart muscle. Therefore, vitamin D may play a role in the pathogenesis of CV problems.[7]
- Gastrointestinal: Due to vitamin D receptors' presence in colon tissues, vitamin D receptors play a role in the proliferation of cells and their response to stimuli. Therefore, a deficiency in vitamin D may play a role in colon cancer. Also as mentioned before, there is a lack of suppression of autoimmune diseases, such as Irritable Bowel Syndrome (IBS) when a vitamin D deficiency is present.[7]
- Psychosocial System: Low levels of vitamin D are associated with depression.[12]
- Integumentary: In the literature, children with burns are at risk of furthering or contracting a vitamin D deficiency and its associated side effects due to low sun exposure. There are no current research has been conducted on adults.[13]
Medical Management [edit | edit source]
Diagnosis: [edit | edit source]
Though vitamin D deficiency is prevalent, vitamin D deficiency screens are not universally supported due to expenses.[18]
- Some clinicians may administer bone decalcification tests via medical imaging and continue with serum testing following results. (Refer to Diagnostic Tests)
- Low vitamin D serum levels are categorized into insufficiency, and the more severe deficiency[20]: Insufficiency 25(OH)D 21-29 ng/mL Deficiency 25(OH)D <20 ng/mL
Due to low availability of foods with adequate vitamin D, treatment is largely based on appropriate supplementation and sun exposure as follows:[20]
Supplimentation Recomendations [edit | edit source]
- Amounts vary depending on cause of deficiency, severity, and physician preference of ramping dosage[14]
- Supplement dosages range from 800 to 1000 IU/d of vitamin D
- Or less than 2000 IU/d to avoid toxicity for those 1 year and old
- Recommended Dietary Allowances (RDA's) for Vitamin D [3]
| Age | Male | Female | Pregnancy |
|---|---|---|---|
| 0-12 months* | 400 IU | 400 IU | |
| 1-13 years | 600 IU | 600 IU | |
| 14-18 years | 600 IU | 600 IU | 600 IU |
| 19-50 years | 600 IU | 600 IU | 600 IU |
| 51-71 yeas | 600 IU | 600 IU | |
| > 70 years | 800 IU | 800 IU |
Physical Therapy Management [edit | edit source]
Physical therapists can take a team approach with medical management through patient education on: Foods high in vitamin D; Importance of following medical recommendations for vitamin D intake; Importance of proper sun exposure with risks of overexposure. A study suggests that implementing a fall treatment protocol comprised of a multidisciplinary team of a Family Medicine (FM) physician, an Internal Medicine (IM) physician, a physical therapist, and a Home Health (HH) nurse leads to more consistent care of elderly patients who experience falls. However, there is a need for reviewing and updating the protocol based on outcomes, and subsequent research is required for improvement in the patient care[21] [21].
There are no direct physical therapy interventions for vitamin D deficiency. Patient will be referred to physical therapy for treatment of impairments that may be a cause of vitamin D deficiency such as decline in muscle strength, decline in physical functioning, or falls prevention. (See Clinical Presentation). In these instances techniques could include:

Falls prevention training eg Otago program, and falls exercise classes
General muscle strengthening exercises
In older adults, there is a blunted responsiveness to resistance training and reduced muscle hypertrophy compared with younger adults. There is evidence that both exercise training and vitamin D supplementation may benefit musculoskeletal health in older adults, and it is plausible that in combination their effects may be additive.[22] Vitamin D deficiency is associated with impaired muscle strength and performance in community-dwelling older people[23].
Dietary Management [edit | edit source]
Adequate Sources of Intake: [edit | edit source]
- D2 (ergocalciferol) is found in vegetable sources and oral supplements
- D3 (cholecalciferol) is obtained primarily from skin exposure to ultraviolet B (UVB) radiation in sunlight, ingestion of food sources such as oily fish and variably fortified foods (milk, juices, margarines, yogurts, cereals, and soy), and oral supplements
Most foods contain between 50 and 200 IU per serving, which varies depending on geographical location and use of th fortification process [6]
| Food | IUs per Serving* | Percent DV** |
| Cod liver oil, 1 tablespoon | 1,360 | 340 |
| Swordfish, cooked, 3 ounces | 566 | 142 |
| Salmon (sockeye), cooked, 3 ounces | 447 | 112 |
| Tuna fish, canned in water, drained, 3 ounces | 154 | 39 |
| Orange juice fortified with vitamin D, 1 cup | 137 | 34 |
| Milk, nonfat, reduced fat, and whole, vitamin D fortified, 1 cup | 115-124 | 29-31 |
| Yogurt, fortified with 20% of the DV of vitamin D, 6 ounces | 80 | 20 |
| Margarine, fortified, 1 tablespoon | 60 | 15 |
| Sardines, canned in oil, drained, 2 sardines | 46 | 12 |
| Liver, beef, cooked, 3 ounces | 42 | 11 |
| Egg, 1 large (vitamin D found in yolk) | 41 | 10 |
| Cheese, Swiss, 1 ounce | 6 | 2 |
IUs= International Units
DV= Daily Values developed by U.S. Food and Drug Administration
Proper sun exposure[3]: [edit | edit source]
- Cloud coverage can decrease absorption by as much as 50%
- Sun through windows is inadequate-Glass blocks the synthesis process
- Sunscreen may block synthesis if over the entire body
- Get 5-30 minutes twice per week between 10AM - 3PM without sunscreen
- Best exposure spots: face, arms, legs, and back
- Tanning beds emit 2-6% UVB (not medically recommended source)
- limit sun exposure without sunscreen to decrease risk of fatal cancers
Differential Diagnosis [edit | edit source]
Fibromyalgia[15] [edit | edit source]
- Myofascial Trigger Points[4]
- Rheumatic diseases[15]
- Polymyositis[4]
- Muscular Dystrophy[4]
Case Report [edit | edit source]
Case Report [24] [edit | edit source]
Authors:
Clement Z, Ashford M, and Sivakumaran
Abstract:
- Vitamin D deficiency is extremely common in multiple myeloma, and it represents a surrogate for clinical multiple myeloma disease status. Patients may complain of dull, persistent, generalized musculoskeletal aches and pains with fatigue or decrease in muscle strength.
- This case highlights that vitamin D deficiency is common in patients with multiple myeloma, and can cause generalized musculoskeletal pain and increase the risk of falls, yet it often goes unrecognized. In patients with non-specific musculoskeletal pain, and inadequate sun-exposure medical practitioners must have a high index of suspicion for vitamin D deficiency.
Patient Characteristics:
- 63 year old man with multiple myeloma
- Current reactivation of herpes zoster
Subjective: Chief complaints include:
- Generalized weakness
- Nonspecific musculoskeletal pain
- Reported multiple falls
Examination:
- Pale presentation with a depressed affect
- Resting tremor, generalized bony tenderness, worse on movement and weight bearing
- Muscle weakness
- Waddling gait
- Bone studies showed features of osteomalacia with a very low Vitamin D level of less than 20 nmol/L
Past Medical History:
- Previously diagnosed with solitary plasmacytoma in 2001, which then progressed to smoldering myeloma in 2004
- 2007 the indolent version of his myeloma transformed to a more aggressive form of myeloma with non-specific musculoskeletal chest pain, anorexia, weight loss, and tumour-lysis requiring hospital admission and plasmapheresis.
- June 2010 the patient was admitted to hospital after multiple falls and zoster reactivation including ophthalmic zoster of the right first and second trigeminal branches.
Intervention:Physical Therapy
Co-intervention:Received 3,000 nmol/L daily of Vitamin D supplementation
Outcomes: 4 months later
- Significant decrease in his generalized musculoskeletal pain
- Bloods showed a normalized level of Vitamin D of 109 nmol/L
- Decrease in alkaline phosphatase to 182 U/L
- Currently undergoing palliative rehabilitation
Resources [edit | edit source]
National Institute of Health
Vitamin D Deficiency: A Surprisingly Common Problem
Top 10 Foods Highest in Vitamin D
References [edit | edit source]
- ↑ 1.0 1.1 1.2 Palacios C, Gonzalez L. Is vitamin D deficiency a major global public health problem?. The Journal of steroid biochemistry and molecular biology. 2014 Oct 1;144:138-45. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4018438/ (last accessed 3.12.2019)
- ↑ Remelli F, Vitali A, Zurlo A, Volpato S. Vitamin D Deficiency and Sarcopenia in Older Persons. Nutrients. 2019 Dec;11(12):2861. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31766576 (last accessed 3.12.2019)
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 Office of Dietary Supplements National Institutes of Health. Dietary Supplement Fact Sheet: Vitamin D. Available at: http://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#ref. Accessibility verified March 28, 2013.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 Goodman C, Fuller K. Pathology: Implications for the Physical Therapist. 3rd ed. Missouri: Saunders Elsevier; 2009.
- ↑ 5.0 5.1 5.2 5.3 5.4 Forrest K, Stuhldreher W. Prevalence and correlates of vitamin D deficiency in US adults. Nutrition Research (New York, N.Y.). January 2011;31(1):48-54. Available from: MEDLINE, Ipswich, MA. Accessed March 29, 2013.
- ↑ 6.0 6.1 6.2 6.3 Kennel KA, Drake MT, Hurley DL. Vitamin D deficiency in adults: when to test and how to treat. Mayo Clin Proc. 2010;85:752–757. quiz 757-8.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 7.13 7.14 Malone R, Kessenich C. Vitamin D deficiency: implications across the lifespan. Journal For Nurse Practitioners [serial on the Internet]. (2008, June), [cited April 2, 2013]; 4(6): 448-454. Available from: CINAHL
- ↑ Turer C, Lin H, Flores G. Prevalence of vitamin D deficiency among overweight and obese US children. Pediatrics [serial online]. January 2013;131(1):e152-e161. Available from: MEDLINE, Ipswich, MA. Accessed March 29, 2013.
- ↑ Olson M, Maalouf N, Oden J, White P, Hutchison M. Vitamin D deficiency in obese children and its relationship to glucose homeostasis. The Journal Of Clinical Endocrinology And Metabolism. January 2012;97(1):279-285.
- ↑ Alzaim M, Wood R. Vitamin D and gestational diabetes mellitus. Nutrition Reviews [serial online]. March 2013;71(3):158-167. Available from: CINAHL with Full Text, Ipswich, MA. Accessed March 29, 2013.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 Prentice A. Vitamin D deficiency: a global perspective. Nutrition Reviews [serial on the Internet]. (2008, Oct 2), [cited March 29, 2013]; 66S153-S164. Available from: SPORTDiscus with Full Text.
- ↑ 12.0 12.1 Högberg G, Gustafsson S, Hällström T, Gustafsson T, Klawitter B, Petersson M. Depressed adolescents in a case-series were low in vitamin D and depression was ameliorated by vitamin D supplementation. Acta Paediatrica (Oslo, Norway: 1992) [serial on the Internet]. (2012, July), [cited March 29, 2013]; 101(7): 779-783. Available from: MEDLINE.
- ↑ 13.0 13.1 Schumann A, Paxton R, Solanki N, Kurmis R, Mackie I, Greenwood J, et al. Vitamin D deficiency in burn patients. Journal Of Burn Care Research: Official Publication Of The American Burn Association [serial on the Internet]. (2012, Nov), [cited March 29, 2013]; 33(6): 731-735. Available from: MEDLINE.
- ↑ 14.0 14.1 14.2 Kulie T, Groff A, Redmer J, Hounshell J, Schrager S. Vitamin D: an evidence-based review. Journal Of The American Board Of Family Medicine: JABFM [serial on the Internet]. (2009, Nov), [cited April 2, 2013]; 22(6): 698-706. Available from: MEDLINE.
- ↑ 15.0 15.1 15.2 Gerber J; Journal of the American Chiropractic Association, 2010 May-Jun; 47 (4): 6-10. (journal article) ISSN: 1081-7166. Accessed 28 March 2013
- ↑ Heidari B, Shirvani J, Firouzjahi A, Heidari P, Hajian-Tilaki K. Association between nonspecific skeletal pain and vitamin D deficiency. International Journal Of Rheumatic Diseases [serial online]. October 2010;13(4):340-346. Available from: Academic Search Premier, Ipswich, MA. Accessed March 28, 2013.
- ↑ van de Luijtgaarden K, Voûte M, Hoeks S, Bakker E, Chonchol M, Verhagen H, et al. Vitamin D deficiency may be an independent risk factor for arterial disease. European Journal Of Vascular And Endovascular Surgery: The Official Journal Of The European Society For Vascular Surgery [serial on the Internet]. (2012, Sep), [cited April 1, 2013]; 44(3): 301-306. Available from: MEDLINE.
- ↑ 18.0 18.1 Gotsman I, Shauer A, Zwas D, Hellman Y, Keren A, Admon D, et al. Vitamin D deficiency is a predictor of reduced survival in patients with heart failure; vitamin D supplementation improves outcome. European Journal Of Heart Failure [serial on the Internet]. (2012, Apr), [cited April 1, 2013]; 14(4): 357-366. Available from: MEDLINE.
- ↑ Lange N, Sparrow D, Vokonas P, Litonjua A. Vitamin d deficiency, smoking, and lung function in the normative aging study. American Journal Of Respiratory Critical Care Medicine [serial on the Internet]. (2012, Oct), [cited April 1, 2013]; 186(7): 616-621. Available from: CINAHL.
- ↑ 20.0 20.1 Holick M. The D-Lightful Vitamin D for Child Health. JPEN J Parenter Enteral Nutr[10.1177/0148607111430189]. 2001 December [cited March 28, 2013]. Available from: http://pen.sagepub.com/content/36/1_suppl/9S.full.pdf+html.
- ↑ 21.0 21.1 Harbison AJ, Prabhu S. Causation and Treatment Algorithms for Elderly Patients who have Fallen in the Twin Tiers.
- ↑ Antoniak AE, Greig CA. The effect of combined resistance exercise training and vitamin D3 supplementation on musculoskeletal health and function in older adults: a systematic review and meta-analysis. BMJ open. 2017 Jul 1;7(7):e014619. Available from: https://www.ncbi.nlm.nih.gov/pubmed/28729308 (last accessed 3.12.2019)
- ↑ Aspell N, Laird E, Healy M, Lawlor B, O'Sullivan M. Vitamin D Deficiency Is Associated With Impaired Muscle Strength And Physical Performance In Community-Dwelling Older Adults: Findings From The English Longitudinal Study Of Ageing. Clinical interventions in aging. 2019;14:1751. Available from: https://www.ncbi.nlm.nih.gov/pubmed/31686797 (last accessed 3.12.2019)
- ↑ Clement Z, Ashford M, Sivakurmaran S. Vitamin D Deficiency in a Man with Multiple Myeloma. N Am J Med Sci. 2011 October; 3(10): 469–471. Available at http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3271427/. Accessed 28 March 2013.
Vitamin D Deficiency And Intrusive Thoughts
Source: https://www.physio-pedia.com/Vitamin_D_Deficiency


Tidak ada komentar:
Tulis komentar